In 2022, my husband and I were blessed with our son Killian. He entered the world early by two months and spent about 11 weeks in the NICU. It was there that Killian was diagnosed with chronic kidney disease. (Read more about the beginning of our journey here.)
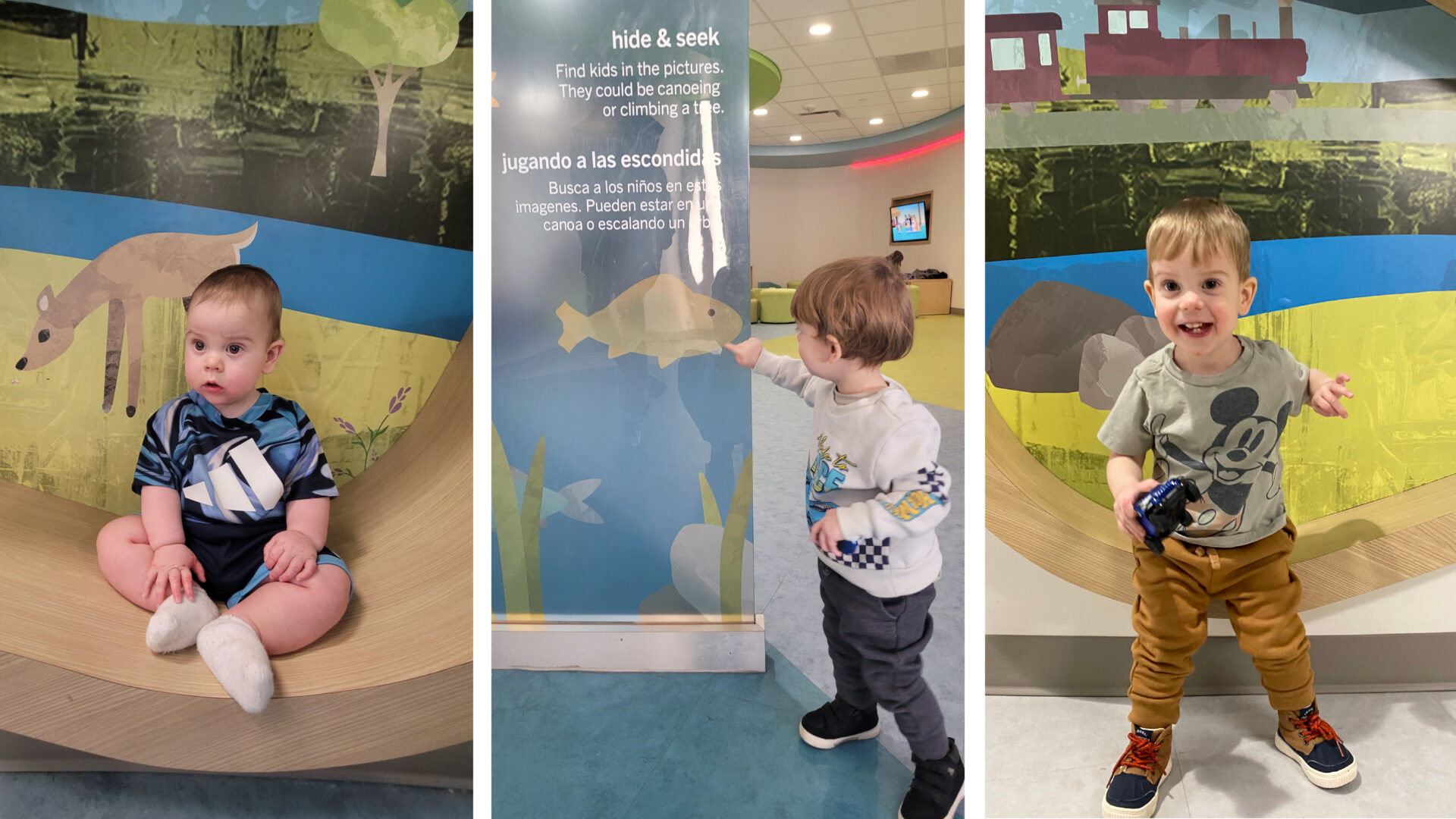
Killian was born with a single, damaged kidney, and in his first nine months, he underwent eight procedures to help improve its function. If you saw Killian today, you’d never know by looking at him how many battles he has fought and won. At two years old, he’s smart, spunky, and full of energy.
What you wouldn’t see are the countless ways our family’s life revolves around managing his condition. There is daily medication, a carefully controlled diet, regular lab work, and occasional ultrasounds to monitor his kidney function. There are the specialist visits—nephrology, urology, neonatology—each playing an important role in keeping him healthy.
For many families of children with chronic illnesses, the calendar isn’t just filled with playdates and milestones; it’s packed with appointments, prescription refills, and long drives to and from different doctors’ offices. And this is where the real challenge begins. Pediatric specialists are rarely under one roof, making care coordination feel like a full-time job. Finding a pharmacy that stocks specialty medications is its own battle. Every appointment means rearranging work schedules, navigating insurance approvals, and hoping for minimal traffic between offices. But most importantly, it means time when our kids cannot simply be kids.
“Dealing with the complexities of a chronic illness in a child is exhausting, burdensome, and impactful for the whole family unit,” agrees Dr. Susan Massengill, Director of Pediatric Nephrology & Hypertension and Pediatric Outpatient Services at Atrium Health’s Levine Children’s Hospital. “Additionally, it is a predictably unpredictable journey with unexpected visits, additional lab work after visits, missed work, missed school and missed opportunities for the “normal” childhood events. Being able to coordinate the care teams is a small gesture to facilitate the medical needs of the child and to make life just a little bit more manageable.”
RECOGNIZING A NEED
Atrium Health saw an opportunity to change this. In 2019, the hospital system approached Little and asked that we study the possibility of moving their pediatric specialty clinics under one roof.
At the time, these clinics were spread across Charlotte and the surrounding areas, forcing families to juggle multiple visits across different locations. In addition to added stress on families, this separation created an additional barrier to collaboration among the various specialty teams. Atrium imagined the benefits of bringing these teams together within one building.
With this in mind, Little and Atrium got to work. We studied which clinics had the most overlap of patients, which specialties worked best together, and which required close access to the adjacent children’s hospital. Beyond the clinics, we looked at the critical support services these teams rely on—pharmacy, lab, imaging—to determine what should be included in the new space. Some specialties volunteered to relocate to make space for those whose co-location would most benefit patients. The goal wasn’t just efficiency—it was to create a better, more connected experience for families and medical teams alike.
From a design perspective, Little’s team focused on both the staff and patient experience. The new space needed to reflect the same innovation and brilliance provided by the specialty clinics, while fostering collaboration and enhancing the established culture of excellence.
From a patient and family perspective, we wanted to design a place that felt playful and age appropriate. When a child requires ongoing medical care throughout their life, the space where they receive that care matters. Fear and anxiety often accompany doctor’s visits, but the right design can help improve each experience. As a parent, there’s no greater reassurance than seeing your child walk into a doctor’s office with wonder and excitement.
TWO WORLDS COLLIDE
In 2023, Killian had his first specialty appointment since being discharged from the NICU. It was a Friday morning, and the brand-new clinic had opened just four days earlier. We were stepping into an unfamiliar chapter of his care—our outpatient journey was just beginning. My husband and I were scared for what the future would bring, and our anxiety was high as we drove to Medical Center Plaza (MCP).
As we stepped off the elevator onto Level Four, we entered a lobby filled with natural light. The walls were covered in beautifully illustrated forest scenes. Every detail had been expertly crafted; from the large tree built into the waiting area to the seating nooks along the walls. My husband took it all in for a moment, then audibly said, “Wow.”
As a member of the design team, I had seen the drawings. I had studied the renderings. I had listened in on countless design discussions and reviews. I understood the design intent. But standing there and seeing the space from my new perspective as a parent with a chronically ill child… in that moment, my husband and I were grateful. Grateful that this space existed. Grateful that our child’s experience had clearly mattered to everyone involved.

The Power of Proximity
MCP became our home base for Killian’s care. Apart from his pediatrician, every specialist he needs is in that building. The pharmacy in the lobby carries his hard-to-find medications. Just steps away, the pediatric lab is staffed by phlebotomists who partner with child life therapists—armed with their bubbles and toys—to distract Killian each time he has to get his blood drawn.
But the real magic of this space isn’t just in its design—it’s in the way it functions. The ease of moving from one specialty to another, the seamless communication between clinics, and the coordinated scheduling that minimizes the burden on patients and families—all of these elements make keeping our children healthy so much easier.
Killian had an appointment with his nephrologist, Dr. Massengill, after one of his surgeries. She was checking in to see how he and his kidney function were doing following the procedure. During the appointment, I mentioned that when I last changed his dressing, I noticed the surgery site looked a bit red. I asked if someone could check it to ensure it wasn’t infected. Since the surgery had been performed by Dr. Keenan in urology, I wasn’t sure if nephrology could address my concern or if I would need to schedule a separate appointment with urology and return another day.
Without hesitation, Dr. Massengill pulled out her phone, called Dr. Keenan, and explained my concern. Dr. Keenan immediately replied that she would be right down.
Fifteen minutes later, she walked into the exam room, looked at Killian’s stitches, and reassured me that everything looked perfect—that slight redness was completely normal.
Had they not been in the same building and so willing to collaborate, Killian and I would have had to make another appointment, come back another day, and spend that time worrying unnecessarily about his healing. On paper, Dr. Keenan simply walking downstairs to see Killian might seem small or insignificant. But for a family constantly navigating appointments, driving to and from clinics, and worrying about every step of recovery, this interaction was a breath of fresh air.
Designing with Deeper Understanding
Throughout this journey, there have been many moments that will forever impact the way I approach my work. I’ve learned that the smallest details—the first impressions, the subtle design choices—can shape how a patient perceives their level of care and safety. I know that distraction in a pediatric waiting room is just as important for the child as it is for the parent anxiously waiting for updates.
More than ever, I recognize the importance of truly understanding how a space will be used and the gravity of the conversations that take place within it. Thoughtful design isn’t just about efficiency—it’s about dignity, about making difficult moments just a little bit easier for the families living them.
This experience has reinforced the power of asking bold questions. What happens when we bring all pediatric specialty clinics under one roof? What barriers can we remove? How can we make care feel seamless rather than overwhelming?
Through design, we may not be able to cure those who are sick—but we can absolutely make their journey easier. And that, in itself, is a kind of healing.

